Apprenticeship Learning Log
Date of Learning: 24th of September 2024
Time: 09:30 – 16:30
Title of learning activity: University learning session
Diary of Learning activity
2024.25 Developing professional and academic skills for Nursing Associates CNR020C112A
Review of learning and recap on topic discussed –
NMC – Mission and Values
The Nursing and Midwifery Council exists to protect the public. We do this by making sure that only those who meet our requirements are allowed to practise as a nurse or midwife in the UK, or a nursing associate in England. We take action if concerns are raised about whether a nurse, midwife or nursing associate is fit to practise. It is against the law to claim to be, or to practise as, a nurse or midwife in the UK, or as a nursing associate in England, if you are not on the relevant part of our register.
It is also a criminal offence for anyone who, with intent to deceive, causes or permits someone else to falsely represent them as being on the register, or makes a false representation about them being on the NMC register.
Publication date: 29 January 2015 Effective from: 31 March 2015 Updated to reflect the regulation of nursing associates: 10 October 2018
A note on this version of the Code
All regulators review their Codes from time to time to make sure they continue to reflect public expectations. This new version of the Code is substantially similar to the 2015 version, but it has been updated to reflect our new responsibilities for the regulation of nursing associates. In joining the register, nursing associates will uphold the Code. The current versions of our Code, standards and guidance can always be found on our website. Those on our register should make sure they are using the most up to date version of the Code.
For more information about the Code, please visit: www.nmc.org.uk/code
Professional standards of practice and behaviour for nurses, midwives and nursing associates. All standards apply within your professional scope of practice.
Introduction
The Code contains the professional standards that registered nurses, midwives and nursing associates must uphold. Nurses, midwives and nursing associates must act in line with the Code, whether they are providing direct care to individuals, groups or communities or bringing their professional knowledge to bear on nursing and midwifery practice in other roles, such as leadership, education, or research.
The values and principles set out in the Code can be applied in a range of different practice settings, but they are not negotiable or discretionary. Our role is to set the standards in the Code, but these are not just our standards. They are the standards that patients and members of the public tell us they expect from health professionals. They are the standards shown every day by those on our register. When joining our register, and then renewing their registration, nurses, midwives and nursing associates commit to upholding these standards. This commitment to professional standards is fundamental to being part of a profession. We can take action if those on our register fail to uphold the Code. In serious cases, this can include removing them from the register.
The NMC Code, its application in developing critical thinking using guidelines and limitations – The NMC Code, 2015 (updated, reviewed and re-published in 2018 to include Nursing Associates)
Developing and applying your critical thinking skills
Critical thinking is not peculiar to academia or nursing practice: people are required to use their critical faculties every day in order to make assessments, judgements and decisions. However, in academic and clinical settings, your critical thinking skills will be under particular scrutiny. You will need to consciously develop your critical thinking skills throughout your study and practice, and you will need to draw on these skills in order to complete academic tasks successfully and develop as a nurse. This will involve a range of skills and abilities which you will have to draw on at different stages of your studies and work:
• problem solving, including discussion of ethical issues;
• decision making;
• applying objective criteria to particular situations;
• reflecting on your nursing practice and on your study skills;
• analysing and evaluating sources of information and ideas in terms of suitability, quality and relevance;
• analysing and evaluating information in order to understand a topic;
• identifying, interpreting and assessing the position of other people;
• identifying, interpreting and assessing the arguments put forward by other people to determine if
– they are well thought through
– they are reasoned and balanced
– they are supported with sound, relevant evidence
– they lead to logical conclusions;
• identifying, interpreting and assessing contrasting points of view;
• evaluating the strength and relevance of the evidence put forward to support different points of view;
• using academic sources to develop your own position (or ‘stance’) in relation to the topics you will investigate, and presenting (or ‘voicing’) this stance in a way that will convince a critical reader;
• developing arguments to support your stance which are well thought through, reasoned and balanced;
• finding sound, relevant evidence to support your arguments.
Critical thinking in nursing practice
Critical thinking is inherent in the NMC Code and you should be guided by the Code in your day-to-day practice. You should also bear the Code in mind, and make reference to it, when discussing nursing practice in academic work. The following sections of the Code are particularly explicit as regards the importance of critical thinking.
Prioritise People – 1 Treat people as individuals and uphold their dignity
1.3 Avoid making assumptions and recognise diversity and individual choice
Practise effectively – 6 Always practise in line with the best available evidence
6.1 Make sure that any information or advice given is evidence-based, including information relating to using any health and care products or services
Practise effectively – 8 Work cooperatively
8.4 Work with colleagues to evaluate the quality of your work and that of your team
Practise effectively – 9 Share your skills, knowledge and experience for the benefit of people receiving care and your colleagues
9.2 Gather and reflect on feedback from a variety of sources, using it to improve practice and performance
Preserve safety – 13 Recognise and work within the limits of your competence
13.1 Accurately assess signs of normal or worsening physical health in the person receiving care
Preserve safety – 19 Be aware of, and reduce as far as possible, any potential for harm associated with your practice
19.2 Take account of current evidence, knowledge and developments in reducing mistakes and the effect of them and the impact of human factors and system failures (Human factors refer to environmental, organisational and job factors, and human and individual characteristics, which influence behaviour at work in a way which can affect health and safety – Health and Safety Executive. You can find more information at www.hse.gov.uk)
Promote professionalism and trust – 20 Uphold the reputation of your profession at all times
20.6 Stay objective and have clear professional boundaries at all times with people in your care (including those who have been in your care in the past), their families and carers
Critical Thinking Skills for your Nursing Degree – Critical Study Skills by Jane Bottomley and Steven Pryjmachuk 1st published in 2018 by Critical Thinking, page 9 – 10 https://www.criticalpublishing.com/asset/208202/1/Critical_Nursing_sample.pdf
The Nursing and Midwifery Council (Publication date: 29 January 2015, Effective from: 31 March 2015, Updated to reflect the regulation of nursing associates: 10 October 2018), https://nmc.org.uk > standards > code > read-the-code-online
Better and safer care for people is at the heart of what we do, supporting the healthcare professionals on our register to deliver the highest standards of care
We value people – we believe they matter
We value fairness – we are consistent and act with integrity
We value transparency – we are open and honest
The purpose of the NMC:
- To protect the public
- To protect professionals
- Considers fitness to practice
- Set and adhere to the Standards in the Code
- Revalidates nurses and midwives
Only those who meet the Code’s requirements are allowed to practise as a Nurse or Midwife, in the UK; or as a Nursing Associate in England
Our roles for 2020–2025: Our strategy is based on three key roles that underpin our purpose: regulate, support, and influence.
Regulate: We promote and uphold high standards, maintain the register of professionals eligible to practise, and step in to investigate on the rare occasions when care goes wrong.
Support: To ensure we regulate as progressively as possible, we proactively support our professions. This allows us to strike the right balance between investigating rare cases of poor practice and promoting excellent practice.
Influence: Regulating and supporting our professions puts us in a unique position to influence the development of health and social care. We work collaboratively with our partners to address common concerns and drive improvement across the sector.
Action taken if concerns are raised about whether a Nurse, Midwife or Nursing Associate is fit to practise:
- Prioritise people
- Practice effectively
- Preserve safety
- Promote professionalism
- Putting patient first
- Communication
- Understand limitations
- Uphold standards
- Respect, kindness and compassion
- Working as a team
- Duty of Candour
- Attitude & behaviour
6Cs of Care – Set of values created through “Compassion in Practice”, a three-year strategy that concluded in March 2016
The 6 Cs of Care – Compassion in Practice: Nursing, Midwifery and Care Staff – Our Vision and Strategy (Department of Health 2012) – A policy document published by the NHS England and developed by (Jane Cummings) then Chief Nursing Officer for England, and (Viv Bennett) Director of Nursing , Department of Health and Lead Nurse, Public Health England.
The three-year strategy set out a shared purpose for nurses, midwives and care staff to deliver high quality, compassionate care, and to achieve excellent health and wellbeing outcomes. Based on the values, pledges and rights set out in the NHS Constitution that patients, the public and staff should and would expect; the strategy was underpinned by six fundamental values designed to support professionals and care staff to deliver excellent care.
Care – Care is our core business and that of our organisations, and the care we deliver helps the individual person and improves the health of the whole Community. Caring defines us and our work. People receiving care expect it to be right for them, consistently, throughout every stage of their life.
Compassion – Compassion is how care is given through relationships based on empathy, respect and dignity – it can also be described as intelligent kindness, and is central to how people perceive their care.
Competence – Competence means all those in caring roles must have the ability to understand an individual’s health and social needs and the expertise, clinical and technical knowledge to deliver effective care and treatments based on research and evidence.
Courage – Courage enables us to do the right thing for the people we care for, to speak up when we have concerns and to have the personal strength and vision to innovate and to embrace new ways of working.
Communication – Communication is central to successful caring relationships and to effective team working. Listening is as important as what we say and do and essential for “no decision about me without me”. Communication is the key to a good workplace with benefits for those in our care and staff alike.
Commitment – A commitment to our patients and populations is a cornerstone of what we do. We need to build on our commitment to improve the care and experience of our patients, to take action to make this vision and strategy a reality for all and meet the health, care and support challenges ahead.
8 Principles of Nursing, what are they? Definition pls…
British Values – Promoting British Values
Definition – The five British Values are the fundamental principles and beliefs that guide the behaviour and interactions of individuals in the United Kingdom. These values have been developed by the UK Government in 2014, with the support of the Department for Education (DfE), in an attempt to create social unity and prevent extremism.
These 5 Values were first outlined in the Prevent Strategy of 2011. The PREVENT Strategy is the UK’s counter-terrorism policy to challenge extremism and terrorism, and part of the UK’s overall counter-terrorism strategy CONTEST. Its objective is to reduce the threat of terrorism by stopping people from becoming terrorists or supporting terrorism. Prevent is one of four stands of the government’s counter-terrorism strategy, along with Prepare, Protect, and Pursue. It focuses on safeguarding vulnerable people from radicalisation and recruitment, and aims to prevent them from being drawn into terrorism and all its forms.
Extract from RMH Learning Hub/Safeguarding Children Level 2 – The Counter-Terrorism and Security Act 2015 contains a duty on specified authorities to have due regard to the need to prevent people from being drawn into terrorism. This is also known as the PREVENT duty.
PREVENT is part of the Government counter-terrorism strategy. It’s designed to tackle the problem of terrorism at its roots, preventing people from supporting terrorism or becoming terrorists themselves.
PREVENT operates in the ‘pre-criminal space’. It is about supporting individuals who are at risk of radicalisation (the process by which a person comes to support terrorism and
extremist ideologies associated with terrorist groups), becoming terrorists or supporting terrorism. It is not about any particular ideology – it covers all forms of extremism.
PREVENT is about:
- Noticing – vulnerability to radicalisation, changes in behaviour, ideology, and other signs of extremist exploitation
- Checking – your concerns out with your line manager to help determine a proportionate response
- Sharing – your concerns, where appropriate, with agencies and as far as possible being open and honest with the individual around your duty to share concerns
These forms of terrorism include:
- Far right extremists
- Al-Qa’ida-influenced groups
- Environmental extremists
- Animal rights extremists
Young people from their teenage years onwards can be particularly vulnerable to getting involved with radical groups through direct contact with members, or increasingly, through the internet. This can put a young person at risk of being drawn into criminal activity and has the potential to cause significant harm – end of extract
The Five British Values are Democracy, Rule of Law, Individual liberty, Mutual Respect, and Tolerance of different Faiths and beliefs.
- Cultures and beliefs of others
- Know that we are special
- Treat everyone equally
- Understand right from wrong
- Try to help others
- Listen and respect others’ opinions
- Understand the consequence of our actions
- Respect the roles of people who help us
Professionalism and its values – The Code contains professional standards RNs, midwives and NAs must uphold in direct care and in leadership, research and education.
Developing professional values and behaviour learning outcomes
Explore professional values underpinning the nurses’ role
Explain the role of the NMC in relation to being an NA and a Nursing student
Discuss the NMC’s role and apply it to your professional practice
Explore the benefits of professional communication via social media
Values – beliefs and views that we hold about what is right or wrong, how it governs one’s own attitude & behaviour to different situations
Group work on defining 5 top values in my life:
Respect for others & mutual respect extended around my individuality & differences (my social background and cultural heritage)
Freedom of speech, freedom of thought to forge my own ideas and opinions
Accountability
Right to live peacefully (right to respect for my private life and family life) which also mirrors national legislation, The Human Rights Article 8: respect for your private life and family life
Importance to acknowledge we are not alone but should aim to live cohesively with others as part of a group (society), though having clearly defined limitations and boundaries
References and additional resources: Staffordshire enquiry (NHS)
About the NMC and Midwifery Council (YouTube)
A guide to undertaking and understanding blood pressure measurement
Blood pressure (BP) measurement is widely recognised as being routine observation that can be used to assess cardiac output and its effectiveness for adequate tissue perfusion (Odell, 2013). Thus, the presence of a BP is a requirement for human existence (Lip and Beevers, 2015). BP measurement, which includes interpreting results and taking appropriate action, is therefore considered a key clinical skill to acquire and maintain, as results can determine the patient care that needs to be delivered (Lister et al, 2021)
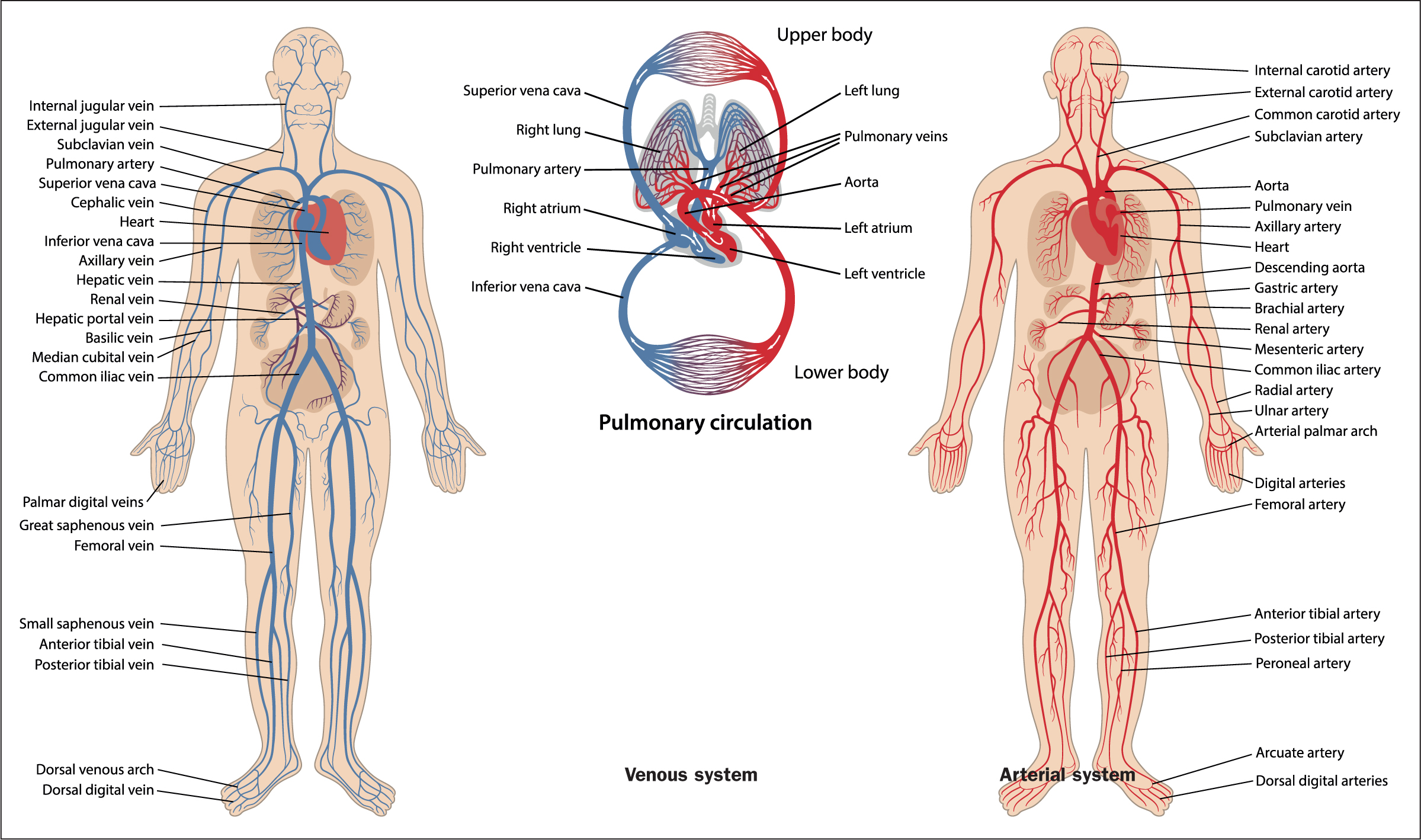
Anatomy and physiology
A BP measurement, in its simplest form, is a determinant of individual cardiac output (the volume of blood pumped out of the heart and into the aorta per minute) and the systematic vascular resistance (the diameter of the arterial blood vessels) (Foley, 2015). To fully understand the process, it is essential that health professionals possess the underpinning knowledge of the anatomy and physiology associated with the cardiovascular system (Figure 1). The cardiovascular system includes the heart, arteries, veins and capillaries and its main function is to distribute blood throughout the body, ensuring that water, nutrients, chemicals, and waste products are exchanged to and from bodily tissues (Boore et al, 2016; Nair, 2017).