Category Archives: Learning Logs: Year 1
Theory hours log sheet July-August 2025
Theory hours log sheet Feb2025 – June2025
Theory Hours Log Sheet Nov24-Feb25
PREVENT Certificate
Learning Log (24.09.25)
Apprenticeship Learning Log
Date of Learning: 24th of September 2024
Time: 09:30 – 16:30
Title of learning activity: University learning session
Diary of Learning activity
2024.25 Developing professional and academic skills for Nursing Associates CNR020C112A
Review of learning and recap on topic discussed –
NMC – Mission and Values
The Nursing and Midwifery Council exists to protect the public. We do this by making sure that only those who meet our requirements are allowed to practise as a nurse or midwife in the UK, or a nursing associate in England. We take action if concerns are raised about whether a nurse, midwife or nursing associate is fit to practise. It is against the law to claim to be, or to practise as, a nurse or midwife in the UK, or as a nursing associate in England, if you are not on the relevant part of our register.
It is also a criminal offence for anyone who, with intent to deceive, causes or permits someone else to falsely represent them as being on the register, or makes a false representation about them being on the NMC register.
Publication date: 29 January 2015 Effective from: 31 March 2015 Updated to reflect the regulation of nursing associates: 10 October 2018
A note on this version of the Code
All regulators review their Codes from time to time to make sure they continue to reflect public expectations. This new version of the Code is substantially similar to the 2015 version, but it has been updated to reflect our new responsibilities for the regulation of nursing associates. In joining the register, nursing associates will uphold the Code. The current versions of our Code, standards and guidance can always be found on our website. Those on our register should make sure they are using the most up to date version of the Code.
For more information about the Code, please visit: www.nmc.org.uk/code
Professional standards of practice and behaviour for nurses, midwives and nursing associates. All standards apply within your professional scope of practice.
Introduction
The Code contains the professional standards that registered nurses, midwives and nursing associates must uphold. Nurses, midwives and nursing associates must act in line with the Code, whether they are providing direct care to individuals, groups or communities or bringing their professional knowledge to bear on nursing and midwifery practice in other roles, such as leadership, education, or research.
The values and principles set out in the Code can be applied in a range of different practice settings, but they are not negotiable or discretionary. Our role is to set the standards in the Code, but these are not just our standards. They are the standards that patients and members of the public tell us they expect from health professionals. They are the standards shown every day by those on our register. When joining our register, and then renewing their registration, nurses, midwives and nursing associates commit to upholding these standards. This commitment to professional standards is fundamental to being part of a profession. We can take action if those on our register fail to uphold the Code. In serious cases, this can include removing them from the register.
The NMC Code, its application in developing critical thinking using guidelines and limitations – The NMC Code, 2015 (updated, reviewed and re-published in 2018 to include Nursing Associates)
Developing and applying your critical thinking skills
Critical thinking is not peculiar to academia or nursing practice: people are required to use their critical faculties every day in order to make assessments, judgements and decisions. However, in academic and clinical settings, your critical thinking skills will be under particular scrutiny. You will need to consciously develop your critical thinking skills throughout your study and practice, and you will need to draw on these skills in order to complete academic tasks successfully and develop as a nurse. This will involve a range of skills and abilities which you will have to draw on at different stages of your studies and work:
• problem solving, including discussion of ethical issues;
• decision making;
• applying objective criteria to particular situations;
• reflecting on your nursing practice and on your study skills;
• analysing and evaluating sources of information and ideas in terms of suitability, quality and relevance;
• analysing and evaluating information in order to understand a topic;
• identifying, interpreting and assessing the position of other people;
• identifying, interpreting and assessing the arguments put forward by other people to determine if
– they are well thought through
– they are reasoned and balanced
– they are supported with sound, relevant evidence
– they lead to logical conclusions;
• identifying, interpreting and assessing contrasting points of view;
• evaluating the strength and relevance of the evidence put forward to support different points of view;
• using academic sources to develop your own position (or ‘stance’) in relation to the topics you will investigate, and presenting (or ‘voicing’) this stance in a way that will convince a critical reader;
• developing arguments to support your stance which are well thought through, reasoned and balanced;
• finding sound, relevant evidence to support your arguments.
Critical thinking in nursing practice
Critical thinking is inherent in the NMC Code and you should be guided by the Code in your day-to-day practice. You should also bear the Code in mind, and make reference to it, when discussing nursing practice in academic work. The following sections of the Code are particularly explicit as regards the importance of critical thinking.
Prioritise People – 1 Treat people as individuals and uphold their dignity
1.3 Avoid making assumptions and recognise diversity and individual choice
Practise effectively – 6 Always practise in line with the best available evidence
6.1 Make sure that any information or advice given is evidence-based, including information relating to using any health and care products or services
Practise effectively – 8 Work cooperatively
8.4 Work with colleagues to evaluate the quality of your work and that of your team
Practise effectively – 9 Share your skills, knowledge and experience for the benefit of people receiving care and your colleagues
9.2 Gather and reflect on feedback from a variety of sources, using it to improve practice and performance
Preserve safety – 13 Recognise and work within the limits of your competence
13.1 Accurately assess signs of normal or worsening physical health in the person receiving care
Preserve safety – 19 Be aware of, and reduce as far as possible, any potential for harm associated with your practice
19.2 Take account of current evidence, knowledge and developments in reducing mistakes and the effect of them and the impact of human factors and system failures (Human factors refer to environmental, organisational and job factors, and human and individual characteristics, which influence behaviour at work in a way which can affect health and safety – Health and Safety Executive. You can find more information at www.hse.gov.uk)
Promote professionalism and trust – 20 Uphold the reputation of your profession at all times
20.6 Stay objective and have clear professional boundaries at all times with people in your care (including those who have been in your care in the past), their families and carers
Critical Thinking Skills for your Nursing Degree – Critical Study Skills by Jane Bottomley and Steven Pryjmachuk 1st published in 2018 by Critical Thinking, page 9 – 10 https://www.criticalpublishing.com/asset/208202/1/Critical_Nursing_sample.pdf
The Nursing and Midwifery Council (Publication date: 29 January 2015, Effective from: 31 March 2015, Updated to reflect the regulation of nursing associates: 10 October 2018), https://nmc.org.uk > standards > code > read-the-code-online
Better and safer care for people is at the heart of what we do, supporting the healthcare professionals on our register to deliver the highest standards of care
We value people – we believe they matter
We value fairness – we are consistent and act with integrity
We value transparency – we are open and honest
The purpose of the NMC:
- To protect the public
- To protect professionals
- Considers fitness to practice
- Set and adhere to the Standards in the Code
- Revalidates nurses and midwives
Only those who meet the Code’s requirements are allowed to practise as a Nurse or Midwife, in the UK; or as a Nursing Associate in England
Our roles for 2020–2025: Our strategy is based on three key roles that underpin our purpose: regulate, support, and influence.
Regulate: We promote and uphold high standards, maintain the register of professionals eligible to practise, and step in to investigate on the rare occasions when care goes wrong.
Support: To ensure we regulate as progressively as possible, we proactively support our professions. This allows us to strike the right balance between investigating rare cases of poor practice and promoting excellent practice.
Influence: Regulating and supporting our professions puts us in a unique position to influence the development of health and social care. We work collaboratively with our partners to address common concerns and drive improvement across the sector.
Action taken if concerns are raised about whether a Nurse, Midwife or Nursing Associate is fit to practise:
- Prioritise people
- Practice effectively
- Preserve safety
- Promote professionalism
- Putting patient first
- Communication
- Understand limitations
- Uphold standards
- Respect, kindness and compassion
- Working as a team
- Duty of Candour
- Attitude & behaviour
6Cs of Care – Set of values created through “Compassion in Practice”, a three-year strategy that concluded in March 2016
The 6 Cs of Care – Compassion in Practice: Nursing, Midwifery and Care Staff – Our Vision and Strategy (Department of Health 2012) – A policy document published by the NHS England and developed by (Jane Cummings) then Chief Nursing Officer for England, and (Viv Bennett) Director of Nursing , Department of Health and Lead Nurse, Public Health England.
The three-year strategy set out a shared purpose for nurses, midwives and care staff to deliver high quality, compassionate care, and to achieve excellent health and wellbeing outcomes. Based on the values, pledges and rights set out in the NHS Constitution that patients, the public and staff should and would expect; the strategy was underpinned by six fundamental values designed to support professionals and care staff to deliver excellent care.
Care – Care is our core business and that of our organisations, and the care we deliver helps the individual person and improves the health of the whole Community. Caring defines us and our work. People receiving care expect it to be right for them, consistently, throughout every stage of their life.
Compassion – Compassion is how care is given through relationships based on empathy, respect and dignity – it can also be described as intelligent kindness, and is central to how people perceive their care.
Competence – Competence means all those in caring roles must have the ability to understand an individual’s health and social needs and the expertise, clinical and technical knowledge to deliver effective care and treatments based on research and evidence.
Courage – Courage enables us to do the right thing for the people we care for, to speak up when we have concerns and to have the personal strength and vision to innovate and to embrace new ways of working.
Communication – Communication is central to successful caring relationships and to effective team working. Listening is as important as what we say and do and essential for “no decision about me without me”. Communication is the key to a good workplace with benefits for those in our care and staff alike.
Commitment – A commitment to our patients and populations is a cornerstone of what we do. We need to build on our commitment to improve the care and experience of our patients, to take action to make this vision and strategy a reality for all and meet the health, care and support challenges ahead.
8 Principles of Nursing, what are they? Definition pls…
British Values – Promoting British Values
Definition – The five British Values are the fundamental principles and beliefs that guide the behaviour and interactions of individuals in the United Kingdom. These values have been developed by the UK Government in 2014, with the support of the Department for Education (DfE), in an attempt to create social unity and prevent extremism.
These 5 Values were first outlined in the Prevent Strategy of 2011. The PREVENT Strategy is the UK’s counter-terrorism policy to challenge extremism and terrorism, and part of the UK’s overall counter-terrorism strategy CONTEST. Its objective is to reduce the threat of terrorism by stopping people from becoming terrorists or supporting terrorism. Prevent is one of four stands of the government’s counter-terrorism strategy, along with Prepare, Protect, and Pursue. It focuses on safeguarding vulnerable people from radicalisation and recruitment, and aims to prevent them from being drawn into terrorism and all its forms.
Extract from RMH Learning Hub/Safeguarding Children Level 2 – The Counter-Terrorism and Security Act 2015 contains a duty on specified authorities to have due regard to the need to prevent people from being drawn into terrorism. This is also known as the PREVENT duty.
PREVENT is part of the Government counter-terrorism strategy. It’s designed to tackle the problem of terrorism at its roots, preventing people from supporting terrorism or becoming terrorists themselves.
PREVENT operates in the ‘pre-criminal space’. It is about supporting individuals who are at risk of radicalisation (the process by which a person comes to support terrorism and
extremist ideologies associated with terrorist groups), becoming terrorists or supporting terrorism. It is not about any particular ideology – it covers all forms of extremism.
PREVENT is about:
- Noticing – vulnerability to radicalisation, changes in behaviour, ideology, and other signs of extremist exploitation
- Checking – your concerns out with your line manager to help determine a proportionate response
- Sharing – your concerns, where appropriate, with agencies and as far as possible being open and honest with the individual around your duty to share concerns
These forms of terrorism include:
- Far right extremists
- Al-Qa’ida-influenced groups
- Environmental extremists
- Animal rights extremists
Young people from their teenage years onwards can be particularly vulnerable to getting involved with radical groups through direct contact with members, or increasingly, through the internet. This can put a young person at risk of being drawn into criminal activity and has the potential to cause significant harm – end of extract
The Five British Values are Democracy, Rule of Law, Individual liberty, Mutual Respect, and Tolerance of different Faiths and beliefs.
- Cultures and beliefs of others
- Know that we are special
- Treat everyone equally
- Understand right from wrong
- Try to help others
- Listen and respect others’ opinions
- Understand the consequence of our actions
- Respect the roles of people who help us
Professionalism and its values – The Code contains professional standards RNs, midwives and NAs must uphold in direct care and in leadership, research and education.
Developing professional values and behaviour learning outcomes
Explore professional values underpinning the nurses’ role
Explain the role of the NMC in relation to being an NA and a Nursing student
Discuss the NMC’s role and apply it to your professional practice
Explore the benefits of professional communication via social media
Values – beliefs and views that we hold about what is right or wrong, how it governs one’s own attitude & behaviour to different situations
Group work on defining 5 top values in my life:
Respect for others & mutual respect extended around my individuality & differences (my social background and cultural heritage)
Freedom of speech, freedom of thought to forge my own ideas and opinions
Accountability
Right to live peacefully (right to respect for my private life and family life) which also mirrors national legislation, The Human Rights Article 8: respect for your private life and family life
Importance to acknowledge we are not alone but should aim to live cohesively with others as part of a group (society), though having clearly defined limitations and boundaries
References and additional resources: Staffordshire enquiry (NHS)
About the NMC and Midwifery Council (YouTube)
A guide to undertaking and understanding blood pressure measurement
Blood pressure (BP) measurement is widely recognised as being routine observation that can be used to assess cardiac output and its effectiveness for adequate tissue perfusion (Odell, 2013). Thus, the presence of a BP is a requirement for human existence (Lip and Beevers, 2015). BP measurement, which includes interpreting results and taking appropriate action, is therefore considered a key clinical skill to acquire and maintain, as results can determine the patient care that needs to be delivered (Lister et al, 2021)
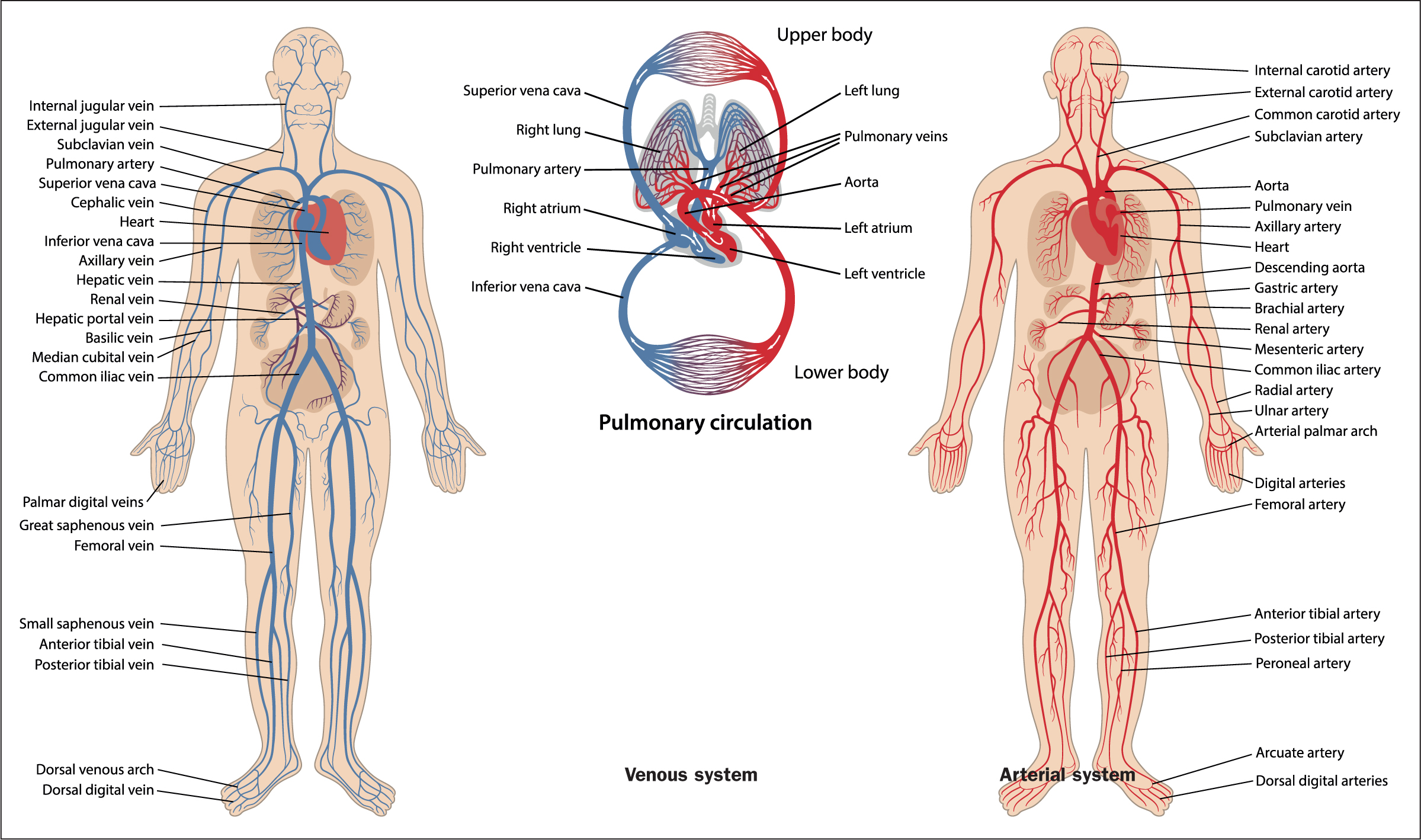
Anatomy and physiology
A BP measurement, in its simplest form, is a determinant of individual cardiac output (the volume of blood pumped out of the heart and into the aorta per minute) and the systematic vascular resistance (the diameter of the arterial blood vessels) (Foley, 2015). To fully understand the process, it is essential that health professionals possess the underpinning knowledge of the anatomy and physiology associated with the cardiovascular system (Figure 1). The cardiovascular system includes the heart, arteries, veins and capillaries and its main function is to distribute blood throughout the body, ensuring that water, nutrients, chemicals, and waste products are exchanged to and from bodily tissues (Boore et al, 2016; Nair, 2017).
Tri-partite review & Theory hours log sheets (September & beg of November)
1st Tri-partite review with line manager on 8th of October 2024
Learning Log Day 5, Week 1 (20.09.2024)
Apprenticeship Learning Log
Date of Learning: 20th of September 2024
Time: 09:30 – 16:30
Title of learning activity: Reflection – Induction & welcome week
Diary of Learning activity
Tri-partites meeting between 07th – 285h of October, to be arranged with line manager & lecturer. To check availability with line manager closer to time, approximately 45 minutes duration.
Uniform issues/replacement – email student@grahamgardner.co.uk
Confirm identity, university, campus course & revision/amendment required
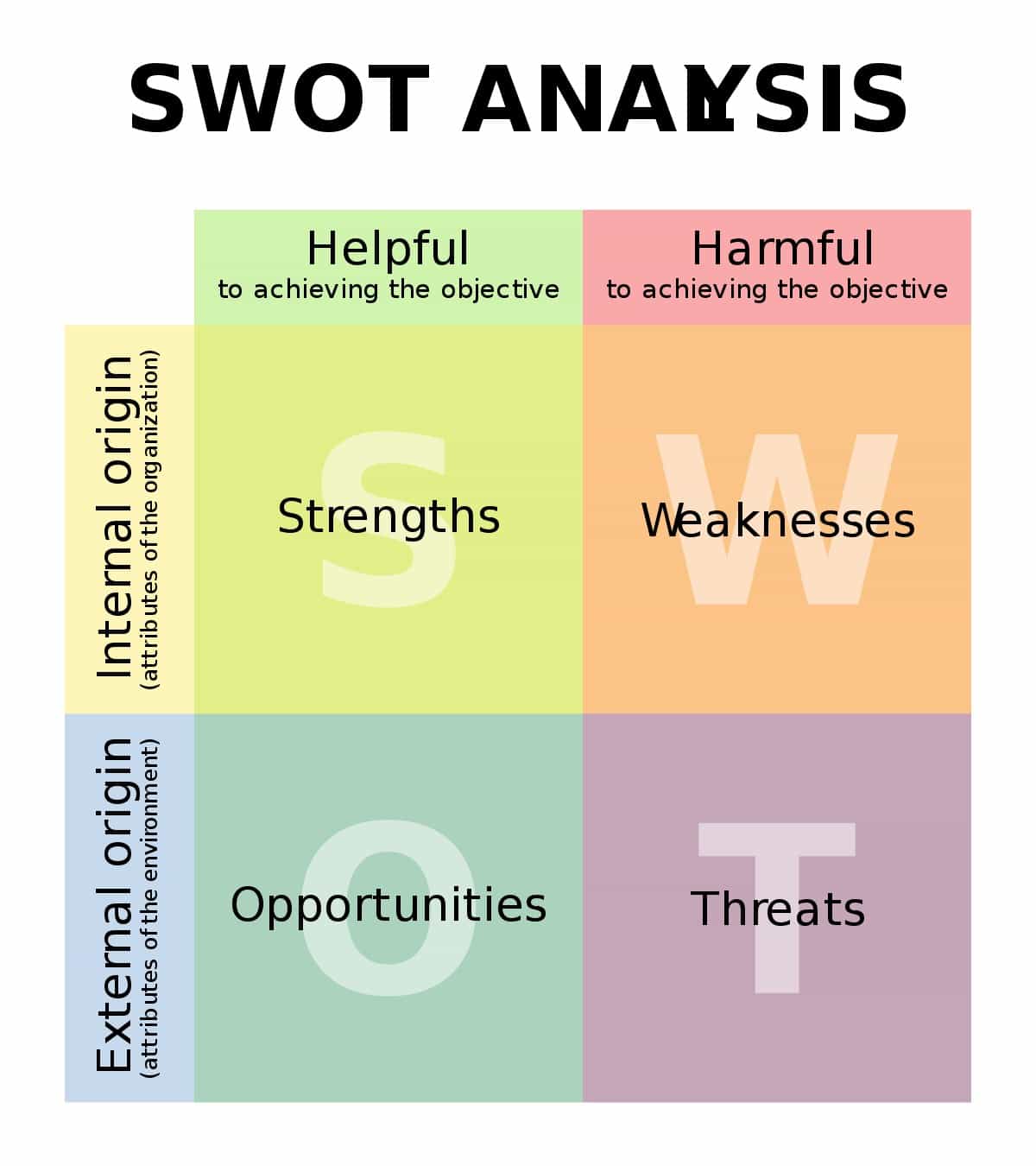
SWOT analysis & SMART objectives – SWOT analysis identifies strength, weakness, opportunities & stress
SWOT is an acronym for Strengths, Weaknesses, Opportunities, Threats. The technique is credited to Albert Humphrey who led a research project at Stanford University in the 1960s and 1970s using data from leading companies involved in long range planning processes.
A SWOT analysis is a planning tool used to understand key factors – strengths, weaknesses, opportunities, and threats – involved in a project or in an organisation. It involves stating the objective of the organisation or project and identifying the internal and external factors that are either supportive or unfavourable to achieving that objective. SWOT is often used as part of a strategic or planning process, but can be applied to help understand an organisation or a situation, and also for decision-making for many different scenarios.
However, while the elements can appear deceptively simple and easy to apply, experience shows that to do a SWOT analysis that’s both effective and meaningful, requires time and a significant resource. Deciding what the strengths and weaknesses of an organisation are, as well as assessing the impact and probability of opportunities and threats, is far more complex than first appears. It requires a team effort and can’t be done effectively by just one person.
A SWOT analysis process generates information that is helpful in matching an organisation or group’s goals, programs, and capacities to the environment in which it operates. The ‘SWOT’ itself is only a data capture exercise – the analysis follows later.
- Strengths: positive tangible and intangible attributes, internal to an organisation and within the organisation’s control
- Weaknesses: internal factors within an organisation’s control that detract from the organisation’s ability to attain the desired goal. Which areas might the organisation improve?
- Opportunities: external attractive factors that represent the reason for an organisation to exist and develop. What opportunities exist in the environment, which will propel the organisation? Identify them by their ‘time frames’.
- Threats: external factors beyond the organisation’s control which could place the organisation mission or operation at risk. The organisation may benefit by having contingency plans to address them if they should occur. Classify them by their severity and probability of occurrence.

S.W.O.T Analysis For Personal Development – Andrew Cussons http://www.andrewcussons.com/s-w-o-t-analysis-for-personal-development/
SWOT ANALYSIS https://www.marketing91.com/swot-analysis/
SMART objectives is a useful guide for setting objectives, specific, measurable, achievable, relevant, time-based. SMART can help when setting new goals for your next appraisal as a way to work on potential plans, ideas to improve, and achieve set goals.

Your objective should clearly state what you or the person needs to achieve. It should include a direction of movement or action, and your objective should describe what needs to be achieved. For example:
- Increase
- Decrease
- Apply
- Change
- Start
- Complete
- Understand
- Improve
Measurable
Your objective should include a measure that shows how you will know the objective has been met or the goal achieved. This measure needs to be tangible, able to be monitored and proof available that the objective has been met or the goal achieved. This could be:
- A KPI (key performance indicator)
- A standard
- A result
- Completion of something
Achievable
The goal or objective must be possible to achieve. Sometimes, you might need to stretch yourself to achieve it, but it should not be impossible.
Realistic
The objective or goal must be realistic in that it is in your realm of responsibility or authority to achieve it. Is it part of your role? Do you have the right authority, responsibility, tools, time and resources to achieve it?
Time-bound
The objective or goal must have a time of when it will be achieved. This can be a fixed point in the future or a reoccurring time if the objective is a regular task you complete as part of your job.
SMART is essentially a checklist you can apply to an objective you have written to ensure it is all of the above and, therefore a SMART objective or a SMART goal.
2024.25 Care delivery 1 (CNR040C115Y) on MOODLE
Oximetry – how does it work? By transmitting light through a finger, it can identify whether oxygen in the blood is at a normal level.
Pulse oximetry is a quick non-invasive monitoring technique that measures the oxygen saturation in the blood by shining light at specific wavelengths through tissue, most commonly the fingernail bed. Deoxygenated and oxygenated haemoglobin absorb light at different wavelengths, 660 nm, and 940 nm, respectively. The absorbed light is processed by a proprietary algorithm in the pulse oximeter to display a saturation value.
In most developed countries, pulse oximetry is the standard of care to monitor oxygen saturation for patients receiving anaesthesia. Pulse oximetry is also used in emergency departments, hospital wards, and ambulances to assess the blood oxygenation in patients with respiratory difficulties or to monitor the potential respiratory depressant effects of pain medications.
Can hypoxia happen with 100% SPO2?
Hypoxia is a condition where the body’s tissues don’t receive enough oxygen. A normal resting oxygen saturation for a healthy individual at sea level is between 95% and 100%. If oxygen saturation level drops below 92%, one should contact a healthcare provider, if it drops to 88% to seek immediate medical attention.
It is possible for hypoxia to happen even at 100% oxygen saturation if exposed to 100% oxygen for a prolonged period of time. Breathing 100% oxygen at normal pressure can lead to acute oxygen poisoning, which can cause symptoms such as:
- Fluid in the lungs
- Hyperventilation or laboured breathing
- Chest pains
- Mild burning on inhalation
- Uncontrollable coughing sometimes with blood
Hypoxemia is a term that describes low levels of oxygen in the blood, specifically within the arterial blood. The condition may indicate a problem with blood circulation or breathing and may present symptoms such as shortness of breath. Hypoxemia can occur for a number of reasons, which can involve underlying medical conditions such as chronic obstructive pulmonary disease (COPD), asthma, and anaemia.
Symptoms of low blood oxygen levels – low blood oxygen levels can result in abnormal circulation and cause the following symptoms, depending on severity:
- Shortness of breath
- Headaches
- Restlessness
- Dizziness
- Rapid breathing
- Chest pain
- Confusion
- High blood pressure
- Lack of coordination
- Visual disorders
- Rapid heartbeat
Causes of low blood oxygen:
- Insufficient oxygen in the air
- An inability of the lungs to inhale and send oxygen to all cells and tissues
- An inability of the bloodstream to circulate to the lungs, collect oxygen, and to transport it around the body
Conditions that can lead to hypoxemia:
Several medical conditions and situations can contribute to the above factors, including:
- Asthma
- Chronic obstructive pulmonary disease (COPD)
- Interstitial lung disease
- Pulmonary hypertension
- Bronchiectasis
- Emphysema
- Acute respiratory distress syndrome (ARDS)
- Pneumonia
- Obstruction of an artery in the lung
- Pulmonary fibrosis, or scarring and damage to the lungs
- Presence of air or gas in the chest that makes the lung collapse
- Excess of fluid in the lungs
People should contact a doctor if they experience:
- Severe and sudden shortness of breath
- Shortness of breath when at rest#
- Severe shortness of breath that worsens during exercise or physical activity
- Irritability or confusion
- A rapid or irregular heartbeat
- Skin discoloration
Vital signs
A healthy human body is able to self-regulate through homeostasis, which is the body’s natural ability to maintain a stable internal environment by correcting abnormal conditions and balancing bodily processes. Vital signs are indicators of the body’s ability to maintain homeostasis.
The four main vital signs routinely monitored by medical professionals and healthcare providers include the following:
- Body temperature
- Pulse rate
- Respiration rate
- Blood pressure
Vital sign measurements are considered important as they measure some of the body’s vital functions and provide necessary information about the patient’s physical wellbeing
The most important aspect of vital signs – heart rate (pulse)
Pulse rate is the number of times the heart beats per minute (bpm). During the cardiac cycle, the pulse is the wave of blood that courses through the body when the left ventricle contracts. After contraction, the heart rests as the cardiac muscle relaxes and the ventricle is filling with blood again. Each pulse beat represents one complete cardiac cycle or one heartbeat – contraction and relaxation.
In a healthy adult, a normal per-minute resting heart ranges from 60 to 100 beats a minute. With physical exertion, the muscles require more oxygen, resulting in an increased heart (pulse) rate and respiration (breathing) rate.
A resting pulse rate above 100 bpm is considered to be a rapid pulse rate, or tachycardia, and a rate below 60 bpm is considered to be a slow pulse rate, or bradycardia
Rhythm refers to the regularity, or equal spacing, of all the beats of the pulse. Normally, the intervals between each heartbeat are of the same duration. A pulse with an irregular rhythm is known as dysrhythmia or arrhythmia. The irregular rhythm may be either a set of random irregular beats or a predictable pattern of irregular beats. An intermittent pulse occurs when the heart occasionally skips a beat. This is not considered abnormal if it does not happen frequently. Exercise or drinking a caffeine-rich beverage may cause this to occur. However, if arrhythmia occurs on a consistent basis, it may indicate heart disease and should be brought to the attention of the physician. If an irregular pulse is detected, the apical pulse should be assessed. The clinician may also order further testing, such as an electrocardiogram (ECG), to further assess the arrhythmia.
Pulse sites – there are 9 areas in the body that allow for easy measurement of the pulse
- Temporal – At side of head just above the ear
- Carotid – At side of neck between larynx and sternocleidomastoid muscle (pulse used in CPR)
- Apical – At apex of heart, left of sternum, 4th of 5th intercostal space below the nipple
- Femoral – In groin where femoral artery passes to leg
- Brachial – Inner (antecubital fossa/space) aspect of the elbow (pulse heard when taking BP)
- Radial – Thumb side of wrist about 1 inch below base of thumb (most frequently used site)
- Popliteal – Behind the knee, pulse located deeply behind the knee and felt where knee is slightly bent)
- Posterior tibial – On medial surface of ankle near ankle bone
- Dorsalis pedis arteries – On top of foot slightly lateral to midline, helps assess adequate blood circulation to the foot
Practical session – pulse check, respiration rate, SPO2
What is SWOT analysis? CIPD https://www.cipd.org/uk/knowledge/factsheets/swot-analysis-factsheet/
The SWOT Framework, CIPD https://www.cipd.org/uk/knowledge/factsheets/swot-analysis-factsheet/
S13: Apply the aims and principles of health promotion, protection and improvement and the prevention of ill health when engaging with people
S14: Promote preventive health behaviours and provide information to support people to make informed choices to improve their mental, physical, behavioural health and wellbeing
S15: Identify people who are eligible for health screening
S16: Promote health and prevent ill health by understanding the evidence base for immunisation, vaccination and herd immunity
S17: Protect health through understanding and applying the principles of infection prevention and control, including communicable disease surveillance and antimicrobial stewardship and resistance
S18: Apply knowledge, communication and relationship management skills required to provide people, families and carers with accurate information that meets their needs before, during and after a range of interventions
S19: Recognise when capacity has changed recognise and how a person’s capacity affects their ability to make decisions about their own care and to give or withhold consent
S20: Recognise people at risk of abuse, self-harm and/or suicidal ideation and the situations that may put them and others at risk
S21: Monitor the effectiveness of care in partnership with people, families and carers, documenting progress and reporting outcomes
S22: Take personal responsibility to ensure that relevant information is shared according to local policy and appropriate immediate action is taken to provide adequate safeguarding and that concerns are escalated
S23: Work in partnership with people, to encourage shared decision making, in order to support individuals, their families and carers to manage their own care when appropriate
S24: Perform a range of nursing procedures and manage devices, to meet people’s need for safe, effective and person-centred care
S25: Meet people’s needs for safety, dignity, privacy, comfort and sleep
S26: Meet people’s needs related to nutrition, hydration and bladder and bowel health
S27: Meet people’s needs related to mobility, hygiene, oral care, wound care and skin integrity
S28: Support people with commonly encountered symptoms including anxiety, confusion, discomfort and pain
S29: Give information and support to people who are dying, their families and the bereaved and provide care to the deceased
S30: Recognise when a person’s condition has improved or deteriorated by undertaking health monitoring, interpreting, promptly responding, sharing findings and escalating as needed
S31: Act in line with any end of life decisions and orders, organ and tissue donation protocols, infection protocols, advanced planning decisions, living wills and lasting powers of attorney for health
S32: Work collaboratively and in partnership with professionals from different agencies in interdisciplinary teams
S33: Maintain safe work and care environments
S34: Act in line with local and national organisational frameworks, legislation and regulations to report risks, and implement actions as instructed, following up and escalating as required
Learning Log Day 4, Week 1 (19.09.2024)
Apprenticeship Learning Log
Date of Learning: 19th of September 2024
Time: 09:30 – 16:30
Title of learning activity: Reflection – Induction & welcome week
Diary of Learning activity
Introduction to Tri-partites – starting in October
Theory hours log – how to log study hours, self-directed study time at work, including training.
Developing professional and academic skills for Nursing Associates CNR020C112A – Developing professional values and behaviours. Introduction to the NMC Code and the 6Cs
The NMC Code – The Code contains the professional standards that registered nurses, midwives and nursing associates must uphold in direct patient care and in leadership, research and education.
The Nursing and Midwifery Council Code: The code represents the professional standards that nurses, midwives and nursing associates must uphold in order to be registered to practise in the UK.
It is structured around four themes – prioritise people, practice effectively, preserve safety, and promote professionalism and trust.
The Code contains a series of statements that taken together signify what good practice by nurses, midwives and nursing associates look like. It puts the interests of patients and service users first, is safe and effective, and promotes trust through professionalism.
“Anyone practising as a registered nurse or midwife in the UK, or a nursing associate in England.”
Their role includes and is not limited to:
Prioritise people – According to the NMC, nursing associates are expected to put the interests of people first. “You make their care and safety your main concern and make sure that their dignity is recognised, assessed and responded to. You make sure that those receiving care are treated with respect, that their rights are upheld and that any discriminatory attitudes and behaviours towards those receiving care are challenged.”
Treat people as individuals and uphold their dignity:
To achieve this, NA must:
- Treat people with kindness, respect and compassion
- Make sure you deliver the fundamentals of care effectively.
- Avoid making assumptions and recognise diversity and individual choice.
- Make sure that any treatment, assistance or care for which you are responsible is delivered without undue delay.
- Respect and uphold people’s human rights.
The fundamentals of care include, but are not limited to, nutrition, hydration, bladder and bowel care, physical handling and making sure that those receiving care are kept in clean and hygienic conditions. It includes making sure that those receiving care have adequate access to nutrition and hydration, making sure that you provide help to those who are not able to feed themselves or drink fluid unaided.
The Registered nursing associate: an overview, Nursing Associates Ian Peate 23 March 2023, British Journal of Nursing, https://www.britishjournalofnursing.com
NMC Nursing and Midwifery Council, https://www.nmc.org.uk/standards/code/
The 6Cs of Care: What they are and what do they mean
The 6Cs core values are considered as qualities and standards all members (irrespective of their position and area of expertise) of any organisation or Trust actively involved in healthcare and working with and around patients are called to identify and relate to as much as possible. Adherence to these values is a guarantee of excellence in the service delivered by nurses and healthcare workers to the public, ensuring service users receive consistent care and support in the different stages of sickness, treatment and end of life or on their path to recovery.
Care is one of the most important qualities required in the health service. The lack of is far more detrimental to the patients; bearing negative impact on the service users, their families and relatives as well as the wellbeing and integrity of staff members failing to provide adequate care or others finding themselves in a constant struggle to maintain a consistent level of service to individuals. Lack of care may result into a high level of complaints and disputes which could negatively affect the corporate /business image of the organisation, whistleblowing to the independent regulator leading to investigation and drastic measures e.g., suspension of services, lawsuits and job losses.
Compassion is defined as “sympathy and concern for the sufferings or misfortunes of others” and is such an important notion one would ideally keep in mind when interacting with patients and individuals, either directly or indirectly affected by sickness and poor health. Compassion allows workers to cement and improve the relationship so much needed between patients and healthcare professionals; it is solely based on the ability to display empathy, provide person-centred care and holistic approach, to respond to the medical and mental health needs of service users. People in need of care are often at their most vulnerable and those close to them are highly sensitive should they perceive care given is not right for their loved ones.
Competence is the state where all (sizeable as an independent individual, part of a team or a larger unit) in employment within any organisation providing healthcare services are able to practise based on the appropriate level of skills and abilities gained through continuous training, positive and result-yielding experience, adherence to agreed ways of working, policies and procedures. Similarly, any organisation working in the patient’s best interest base their treatment and research on the use of appropriate equipment, technology, proper settings & environment, up-to-date clinical and latest technological knowledge.
Communication is essential in the early stages of establishing contact with the patient and their close ones, to help gain their trust, garner essential information on their medical condition (patient history) and how it could be affecting their quality of life. Moreover, appropriate and respectful communication would involve active listening, making sure the patient or their advocate/next of kin is supported and involved in the decision-making process around their care and treatment in line with the Mental Capacity Act, so as to reach a mutual understanding and agreement. Communication is also important across healthcare professionals and medical teams to ensure treatment and care is delivered efficiently in the service user’s best interest.
Courage is to muster the strength and will to stand out against malpractice and to speak up where legitimate concerns should the health and wellbeing of both patients and staff members alike is at risk. It also takes courage and requires resilience for healthcare workers to stay open-minded and willing to abandon safety of limited perception, at times considered as misleading outdated views, and obsolete methods to keep up with everchanging and innovative ways of working.
Commitment is going that extra mile and beyond for those in need of lifesaving care, irrespective of their characteristics in such a way that all patients can be treated without bias, commitment is both a personal and team effort dedicated to maintain or improve the care and experience of all our patients
What does professionalism mean to you?
The definition of professionalism is the combination of all the qualities connected with trained and skilled people, where an individual is dictated to conduct oneself with responsibility, integrity, accountability and excellence.
In a clinical setting/environment, professionalism reflects on an individual’s behaviour at work, in their job role and interaction with service users and staff members alike. It is applying and promoting agreed policies and procedures in their daily activities, encouraging their peers to remain focused on SOPs, and agreed ways of working, ability to show accountability for their actions and to explain the rationale for their initiatives, promoting integrity, workplace values and mission.
Professionalism is following national guidance and legislation, working in towards:
Promoting and respecting protected characteristics under the Equality Act 2010
Dignity and confidentiality, safeguarding and initiating measures to protect vulnerable individuals – reporting and escalating as required.
Whistleblowing and challenging discrimination, direct or indirect as well as practices putting oneself and others at risk.
Not engaging or coercing in activities that are not within their competence and skills.
Respecting and using the organisation’s resources effectively
Always maintaining an acceptable attitude at work, friendly while maintaining healthy boundaries with patients/public/visitors/colleagues, refrain from engaging in gossiping, adhering to the dress code at work, allowing others to engage and express their point of view (ideas, feelings, distress) with good communication and listening skills, showing their understanding and attentive to their own body language as well as others.
Introduction to module on Tuesday 24.09.2024
Principles of academic writing – Wednesday 25.09.2024
KSBs addressed:
K1: Understand the Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC, 2018), and how to fulfil all registration requirements
K2: Understand the demands of professional practice and demonstrate how to recognise signs of vulnerability in themselves or their colleagues and the action required to minimise risks to health
K7: Understand the importance of courage and transparency and apply the Duty of Candour
K24: Know how to support people with commonly encountered symptoms including anxiety, confusion, discomfort and pain
K31: Understand how inadequate staffing levels impact on the ability to provide safe care and escalate concerns appropriately
K33: Understand when to seek appropriate advice to manage a risk and avoid compromising quality of care and health outcomes
S1: Act in accordance with the Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC, 2018), and fulfil all registration requirements
S2: Keep complete, clear, accurate and timely records
S3: Recognise and report any factors that may adversely impact safe and effective care provision
S4: Take responsibility for continuous self-reflection, seeking and responding to support and feedback to develop professional knowledge and skills
S6: Act as an ambassador for their profession and promote public confidence in health and care services
S7: Communicate effectively using a range of skills and strategies with colleagues and people at all stages of life and with a range of mental, physical, cognitive and behavioural health challenges
S8: Recognise signs of vulnerability in self or colleagues and the action required to minimise risks to health
S9: Develop, manage and maintain appropriate relationships with people, their families, carers and colleagues
S10: Provide, promote, and where appropriate advocate for, non-discriminatory, person-centred and sensitive care at all times, reflecting on people’s values and beliefs, diverse backgrounds, cultural characteristics, language requirements, needs and preferences, taking account of any need for adjustments
S11: Report any situations, behaviours or errors that could result in poor care outcomes
S12: Challenge or report discriminatory behaviour
S14: Promote preventive health behaviours and provide information to support people to make informed choices to improve their mental, physical, behavioural health and wellbeing
S24: Perform a range of nursing procedures and manage devices, to meet people’s need for safe, effective and person-centred care
S25: Meet people’s needs for safety, dignity, privacy, comfort and sleep
S28: Support people with commonly encountered symptoms including anxiety, confusion, discomfort and pain
S30: Recognise when a person’s condition has improved or deteriorated by undertaking health monitoring, interpreting, promptly responding, sharing findings and escalating as needed
S33: Maintain safe work and care environments
S34: Act in line with local and national organisational frameworks, legislation and regulations to report risks, and implement actions as instructed, following up and escalating as required
S36: Respond to and escalate potential hazards that may affect the safety of people
S42: Support, supervise and act as a role model to nursing associate students, health care support workers and those new to care roles, review the quality of the care they provide, promoting reflection and providing constructive feedback
B1: Treat people with dignity, respecting individual’s diversity, beliefs, culture, needs, values, privacy and preferences
B2: Show respect and empathy for those you work with, have the courage to challenge areas of concern and work to evidence based best practice
B3: Be adaptable, reliable and consistent, show discretion, resilience and self-awareness
Learning Log Day 3, Week 1 (18.09.2024)
Apprenticeship Learning Log
Date of Learning: 18th of September 2024
Time: 09:30 – 16:30
Title of learning activity: Reflection – Induction & welcome week
Diary of Learning activity
ePortfolio – Explored learning platform, logging into ePortfolio for posting daily learning logs, self-directed learning, e-certificates, essays and assignments.
Artificial intelligence (AI) – open discussion on AI, its contribution/application in building essays. We are reminded to maintain integrity and refrain from relying on AI in our work.
Anatomy and Physiology (A & P) – Introduction to anatomy and physiology. The aim is to provide an overview of the body’s systems, types of cells and the concept of homeostasis.
Learning in class today:
2024.25 Understanding health and illness across the lifespan – CNR020C111A
- Introduction to A&P: Systems, Cells and Homeostasis (Understanding Health and Illness)
Aim of the session:
To provide an overview of body systems, types of cells, information on homeostasis and how the body maintains homeostasis
Familiarise with common anatomical terms, locations/positions (directional terms)
Learning outcomes:
- Anatomical position
Standing upright
Forward facing
Arms at the side
Palms forward
Feet parallel
- Positional terms – body parts are described relative to other parts
Superior – toward the top or head region
Inferior – toward the bottom or feet
Anterior or Ventral – towards the front of the body
Posterior or Dorsal – towards the back of the body
Medial – closer to the midline
Lateral – farther from midline
Proximal – body part is closer to the point of attachment than other body part
Distal – body part further from point of attachment than other body part
Superficial – closer to the surface
Deep – deeper in the body
- Body cavities and regions
Learning using body cavities to help organise the different organs and organ systems provides a useful way for breaking down information into more manageable components. Body cavities represent fluid filled spaces which house and protect the major internal organs
Dorsal body cavity – cranial & vertebral cavity
Ventral body cavity – thoracic, abdominal & pelvic cavity
Distal – in anatomy, distal means a part of the body is farther away from the centre of the body than another part, e.g., the hand is distal to the shoulder
Proximal – means situated nearest to the point of attachment or origin
The abdomen is divided into 4 quadrants – right, left, upper, lower
The abdomen is sub-categorised in 9 regions – right hypochondriac region, epigastric region, left hypochondriac region, right lumbar region, umbilical region, left lumbar region, right iliac region (where the appendix is located), hypogastric region, left iliac region
- Regions of the body
Head, neck, trunk, upper limbs, hands, lower limbs, feet
- Leads of organisation
Organisation in anatomy refer to the hierarchy within biological systems, starting from cellular level, to tissue level, organ level, organism level.
Each level as follows:
- Chemical level – the smallest layer of structural organisation, the body is made up of various chemicals. Different chemicals combine to form the various molecules found in the human body. Atoms combine to form molecules. E.g., Adenosine triphosphate (ATP – is the source of energy for use and storage at the cellular level; used for various cellular functions including transportation of different molecules across cell membranes, and other functions include supplying energy required for muscle contraction, neurotransmission, DNA and RNA synthesis), oxygen, carbon dioxide, hydrogen. The importance of electrolytes – electrolytes are chemicals that conduct electricity when dissolved in water. They regulate nerve and muscle function, hydrate the body, balance blood acidity and pressure, and help rebuild damaged tissue.
- Cellular level – cells are the smallest units of the living organisation and are the building blocks of the human body. The human body develops from a single cell, the zygote, a fertilised egg cell that results from the union of a female gamete (egg, or ovum) with a male gamete (sperm). In the embryonic development of humans and other animals, the zygote stage is brief and is followed by cleavage, when the single cell becomes subdivided into smaller cells.
- Tissue level – collections of similar cells grouped together to perform a specific function. Tissues consist of similar types of cells. E.g., nervous tissue, muscular tissue, epithelial tissue, connective tissue
- Organ level – structures that operate to perform a specific function; and consist of two or more types of tissue, which enable them to perform a specific role or function. E.g., the heart, lungs, liver, kidneys, the skin
- Organ system level – a group of organs that work collaboratively to perform specific functions. E.g., the skeletal system, the muscular system, the circulatory system, the respiratory system, the nervous system, the endocrine system, the digestive system, the urinary system, the reproductive system
- Organism level – a living form where all the other body structures function to bring life to the organism. E.g., humans, mammals, reptiles
The human cell structure and it cell components – DNA and genes, the cell membrane and transport
Passive transport is the movement of molecules across a cell membrane without the use of energy. It occurs when molecules move from an area of high concentration to an area of low concentration, which is known as moving down a concentration gradient. There are several types of passive transport:
Diffusion – small nonpolar molecules, like oxygen and carbon dioxide, move through the membrane by diffusion
Osmosis – water molecules move through a semi-permeable membrane from an area of high water concentration to an area of low water concentration
Facilitated diffusion – large, insoluble molecules, like glucose or amino acids, move through the membrane with the help of carrier proteins or pores in the membrane
Active transport – the process of moving molecules across a cell membrane from an area of low concentration to an area of high concentration, This process is against the concentration gradient and requires energy. Examples of active transport:
The uptake of glucose by the epithelial cells in the small intestines and the uptake of ions from soil water by roots hair cells in plants
Sodium-potassium pump – a transport of protein that moves sodium out of cells and potassium into cells. This process helps nerve cells transmit nerve impulses
The smallest structures capable of performing activities essential for life. Cells are made up of molecules. E.g., muscle cells, nerve cells, blood cells
- Homeostasis/haemodynamic
The body’s many functions, beginning at cellular level, operate as to not to deviate from a narrow range of internal balance, a state known as dynamic equilibrium, despite changes in the external environment. Those changes in the external environment alter the composition of the extracellular fluid surrounding the individual cells of the body, but a narrow range must be maintained to stave off death of cells, tissues, and organs. In short, the purpose of homeostasis is to maintain the established internal environment without being overcome by external stimuli that exist to disrupt the balance.
2 physiological responses:
- Shivering and arrector pili muscle – shivering is a remarkable thermogenic response in homeothermic animals, including humans, that involves rapid, repeated skeletal muscle contractions leading to heat production through the inefficiency of ATP utilisation. Shivering maintains homeostasis when the body gets too cold by generating heat.
- The erector pili muscle, also known as the arrector pili muscle or pilomotor muscle, is a hair-supporting dermal tissue and a king of smooth muscle in the skin that causes hair to stand, and maintain the warmth of the mammalian body through erecting hairs.
5 essentials for survival:
- Water
- Oxygen
- Nutrients
- Normal body temperature
- Normal blood pressure
Characteristics of life:
- Movement
- Respiration
- Sensitivity
- Growth – increase in the size or number of cells
- Reproduction
- Excretion
- Nutrition
With the help of reading material on MOODLE, information will help me familiarise myself with the clinical terms above towards assessment (mock & exam) in February 2025. Additionally, knowledge of terms and general functions will, in my role as a student nursing associate, support patients with their health and well-being, and to identify and document patient’s clinical information (body maps including pressure sores and wounds, compromised skin integrity, pain sites & locations) appropriately.
In the course of my duties and responsibilities at work, while performing physiological measurements, I was able to identify a mild muscular spasm in the left hypochondrial region alongside pain scoring system, and other chest discomfort the patient was experiencing. Upon recording detailed information, clinician was able to initiate further investigation (ECG) to establish primary risk or indication of heart failure.
Assignment for home:
To complete online questionnaire on VARK
To upload care certificate on ePortfolio
Check session resources on MOODLE, module outline and learning outcomes.
Essential reading – anatomy book list on MOODLE
Self-directed learning and research – definition and difference between “acidotic”, “alkalotic” – acidosis and alkalosis are conditions that occur when the body’s pH levels are abnormal:
- Acidosis occurs when the body’s pH levels drop below 7.35, indicating too much acid in the body’s fluids. Symptoms include fatigue, confusion, nausea and vomiting, headaches, increased breathing rate and depth, seizures, and coma.
- Alkalosis occurs when the body’s pH levels rise above 7.45, indicating too much base in the blood. Symptoms include irritability, weakness, cramping, muscle twitching, muscular spasms, fatigue, confusion, tremor, tingling and numbness, abnormal heart rate (arrhythmia), and seizures
- Why is dangerous to administer oxygen to a COPD patient?
Oxygen therapy can be dangerous for patients with chronic obstructive pulmonary disease (COPD) if not properly prescribed and monitored.
NICE (2016) Quality statement 6: Emergency oxygen during an exacerbation (a sustained worsening of a person’s symptoms from their stable state beyond usual day-to-day variations and is an acute onset, commonly reported symptoms are worsening breathlessness, cough, increased mucus production, and a change in the colour of the mucus) – people receiving oxygen for an acute exacerbation of chronic obstructive pulmonary disease (COPD) have their oxygen saturation levels maintained between 88% and 92%.
During an exacerbation, people with COPD may experience a worsening of gas exchange in the lungs, which can lead to low blood oxygen levels. Emergency oxygen is often given during the treatment of an exacerbation, either in the community, during transfer to hospital in an ambulance or while being assessed at hospital.
In some people, uncontrolled oxygen therapy may reduce the depth and frequency of breathing, leading to a rise in blood carbon dioxide levels and a fall in the blood pH (acidosis). Controlled oxygen therapy must therefore be administered by a delivery device and at a flow that helps the oxygen saturation to be maintained between 88% and 92%.
KSBs addressed:
K1: Understand the Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC, 2018), and how to fulfill all registration requirements
K4: Understand the principles of research and how research findings are used to inform evidence-based practice
K10: Understand the principles of epidemiology, demography, and genomics and how these may influence health and well-being outcomes
K16: Understand body systems and homeostasis, human anatomy and physiology, biology, genomics, pharmacology, social and behavioural sciences as applied to delivery of care
S1: Act in accordance with the Code: Professional standards of practice and behaviour for nurses, midwives and nursing associates (NMC, 2018), and fulfil all registration requirements
S2: Keep complete, clear, accurate and timely records
S5: Safely demonstrate evidence-based practice in all skills and procedures required for entry to the register: Standards of proficiency for nursing associates Annex A & B (NMC 2018)
S17: Protect health through understanding and applying the principles of infection prevention and control, including communicable disease surveillance and antimicrobial stewardship and resistance
S24: Perform a range of nursing procedures and manage devices, to meet people’s need for safe, effective and person-centred care
S35: Accurately undertake risk assessments, using contemporary assessment tools
S36: Respond to and escalate potential hazards that may affect the safety of people
S44: Access, input, and apply information and data using a range of methods including digital technologies, and share appropriately within interdisciplinary teams
B1: Treat people with dignity, respecting individual’s diversity, beliefs, culture, needs, values, privacy and preferences
K16: Understand body systems and homeostasis, human anatomy and physiology, biology, genomics, pharmacology, social and behavioural sciences as applied to delivery of care
S2: Keep complete, clear, accurate and timely records
S30: Recognise when a person’s condition has improved or deteriorated by undertaking health monitoring, interpreting, promptly responding, sharing findings and escalating as needed
